|
.....there is nothing more
difficult to arrange, more doubtful of success, and more
dangerous to carry through than initiating changes ... The
innovator makes enemies of all those who prospered under the old
order, and only lukewarm support is forthcoming from those who
would prosper under the new. Their support is lukewarm partly
from fear of their adversaries . . . and partly because men are
generally incredulous, never really trusting to new things
unless they have tested them by experience.
Machiavelli, II
Principe 1
The
nature and outcome of the 1974 reorganisation of the National
Health Service can only be touched upon briefly here. It was
planned by a Conservative administration as part of the
government’s wider programme of administrative reform, which
aimed to make it easier to plan and develop services across
authority boundaries and to give scope for changing the balance
of resource allocation between them. Just before the date of
reorganisation a general election brought Labour to power. Mrs
Barbara Castle became Secretary of State for Social Services in
March 1974 and Dr David Owen, Minister of State for Health. Some
features of the reorganisation did not appeal to the new
administration but the central aim of unifying community and
hospital services was accepted as sound.
Reorganisation had a number of objectives. First was the
unification of the three parts of the NHS, hospital services,
family practitioner services and the health services provided by
local authorities, into a single structure. Second, the new
structure was expected to make easier a ‘clear definition and
allocation of responsibilities, with maximum delegation
downwards matched by accountability upwards’. Third, there was
to be a comprehensive planning system to ensure that policies
were translated into action.2 Though the
changes in 1974 can now be viewed as no more than a single stage
in the evolution of the health service system, it seemed a vast
step to those working in London hospitals. With the exception of
the postgraduates, the teaching hospitals lost their boards of
governors, and hospital management committees disappeared. Newly
created area health authorities and health districts served a
defined population. They advertised for staff and many familiar
faces disappeared from the hospitals, either by success in the
competition for the new jobs or by early retirement.
The
‘Grey Book’ on management arrangements for the reorganised
health service was the outcome of a study supervised by a
committee whose members were drawn from the three branches of
the service and the Department, chaired by its permanent
secretary, with the assistance of McKinsey and Co and the Health
Services Organisation Research Unit of Brunel University.3 Roles
and responsibilities were defined with a precision not to
everybody’s liking. The concept of management by consensus among
chief officers of different disciplines was introduced. With
few exceptions the officers of the regional health authorities
were those of the old regional hospital boards; they had many
new things to learn. Health authorities now had a wider span of
responsibilities, ranging from community health services to the
regional specialties and the high technology of teaching
hospitals. Authority meetings were now to be held in public and
the membership of area health authorities included four nominees
of local authorities. Each health district related to a new
consumer organisation, the community health council, which had a
right to be consulted on changes in service and to oppose
significant alterations at ministerial level.
These organisational changes were carried out against a
background of increasing stringency and the new structure was
sometimes blamed for problems which were really caused by a
shortage of money, particularly in London. There was widespread
if spasmodic industrial action by many groups of staff. The
teaching hospitals had difficulty in adjusting to the new order,
and regretted the now distant relationships with the Department
of Health and Social Security. Two were in the process of
relocation, Charing Cross in Fulham and the Royal Free in
Hampstead. Neither believed that the cost of running the new and
larger facilities had been estimated correctly.
Medicine was not standing still. Diagnostic imaging was being
revolutionised, ultrasound was developing and the first computer
assisted scanners were being introduced into London hospitals.
New methods of treatment were developed, often pioneered in the
teaching hospitals but sometimes being introduced into the
practice of district general hospitals. Coronary artery surgery
and pacemaker insertion was expanding rapidly; oncology, bone
marrow transplantation and joint replacement also had to find
their place amongst the services offered, and had to be
financed. Services for the elderly, the mentally ill and
mentally handicapped also needed improvement. These ‘Cinderella
services’ were now unambiguously the responsibility of the same
district authorities as were the teaching hospitals. They
therefore came into direct conflict with new initiatives in
acute treatment, within the same budget.
Planning and
finance
The
introduction of a comprehensive planning system involving the
Department of Health, the regions, the areas and the districts,
was intended to be an essential component of the 1974
reorganisation. Nowhere was it more important than in London
with its legacy of problems. The deficiencies in primary care
and long stay services, the concentration on acute services, and
the problem of reconciling London’s role in medical education
with the level of acute facilities likely to be available in the
future remained unresolved.
The ‘Grey Book’ outlined the nature
of the health service planning system and a few regions like
North East Thames implemented it. Two years after
reorganisation, in 1976, a guide to the NHS
Planning System and a consultative document on Priorities
for Health and Personal Social Services in England were
issued to launch it more widely.4 Planning
was now to be based upon the requirements of different ‘client’
groups, rather than proposals for capital developments at
individual hospitals. It was also to take place within realistic
resource assumptions. Here was a problem; the then current
proposals for building far exceeded the funds likely to be
available. Costs had often escalated and the new regional health
authorities had the unhappy task of informing some hospitals
that long-cherished developments were unlikely to come to
fruition for many years to come.
In London even existing services
were under threat. From 1977/8 regional authorities received
allocations which reflected the decision to re-distribute
revenue in line with the recommendations of the Resource
Allocation Working Party (RAWP).5 This
proposed that the money available to a region should primarily
reflect the size of its population, weighted by standardised
mortality ratios and other factors, rather than the costs of
services currently provided or its historic funding. On this
basis the discrepancies between regional allocations were
considerable. Target allocations, the money which a region would
receive if equity ruled, were calculated. The four Thames
regions were considerably ‘over-target’ and their financial
growth rate would now be below national average. Simultaneously
the Thames regions were expected to redress their own internal
inequalities and deficiencies in service. Some areas were far
better funded than others and hospitals like The London realised
that they would have to lose money to Essex, or to groups like
the mentally ill whose conditions required urgent improvement.
The compounding effects of national and regional reallocation
and the demands of the long stay specialties made the financial
position of the allegedly over-funded central London teaching
districts, and the continuing development of high technology
medicine, look bleak. The University of London and its medical
schools rapidly appreciated the
potential effect upon acute hospital services and medical
education, and established a working party to look at the
position.
The financial pressures upon
teaching districts were now clear but the speed with which they
could react was reduced by the need for public consultation, and
local opposition to any reduction in health services. Some of
the districts with the greatest financial problems were matched
by local authorities which were left-wing in complexion. Their
nominees on the area health authorities made it clear that any
reductions were anathema to them. One teaching area, Lambeth,
Southwark and Lewisham, passed a resolution in 1979 that in
effect limited the extent to which it was prepared to cut
clinical services. This action would inevitably have led the
authority to exceed the cash limit it received. Mr Patrick
Jenkin, the Secretary of State, appointed commissioners under
section 86 of the NHS Act 1977, which permitted him to give
directions for a specific period to ensure, in an emergency,
that services would continue to be available. This decision was
subsequently challenged successfully, but not before a measure
of financial control had been re-established. The court ruled
that Mr Jenkin had acted outside the power of the section by
failing to specify the duration of the crisis. Instead, the
court said, he might have acted under section 17, directing the
authority to economise in specific terms.6
Planning in
London
The
forty years preceding the 1974 reorganisation had seen major
demographic changes and the removal and rehousing of many
Londoners in new towns as an act of policy. The population of
inner London had fallen, faster indeed than the planners had
expected, from 4,397,000 in 1931 to 2,772,000 in 1971. The
number of acute hospital beds in central London had fallen
somewhat, but the proportion compared with the residential
population had risen.
When the figures from the joint survey carried out in 1931 by
the Voluntary Hospitals Committee and the London County Council7 are
compared with hospital statistics for the same listed hospitals
in 1973 (where they were still in operation) the number of beds
in teaching hospitals has risen, mainly as result of post-war
reconstruction at a larger size. Beds in specialist hospitals
fell, largely because small hospitals for women and children had
closed or been incorporated into general teaching hospitals. The
capacity of the old municipal hospitals had fallen partly as a
result of war damage and partly because some very large
hospitals were reduced in size, while some fever hospitals like
the Brook in Woolwich and the Grove in Tooting had been
converted into general hospitals or specialist units. Patients
with acute illnesses were well served, but the position of the
elderly and the mentally ill was less favourable.
Services for these long stay patients were generally provided in
old buildings, sometimes miles from where they had lived. The
changing demography of London called for a different and leaner
pattern of hospital service in central London, although the
process of slimming down was complicated by the need to provide
clinical facilities for the progressively expanding medical
student intake.
Acute beds
available in the same hospitals in 1931 and 1971
| |
1931 |
1971 |
% change |
| Teaching
hospitals |
5,672 |
7,260 |
+ 36 |
| Special(ist)
hospitals |
5,617 |
4,887 |
-13 |
| General,
below 100 beds |
442 |
445 |
+ 0.7 |
| General,
above 100 beds |
2,330 |
2,561 |
+ 10 |
| |
14,151 |
15,153 |
|
| LCC
hospitals appropriated |
16,920 |
9,536* |
- 38 |
| |
31,071 |
24,689 |
- 20 |
| |
7.06/1000
resident population. |
8.9/1000
resident population |
|
*To this figure
one might add beds in hospitals which provided fever services in
1931, but had become general hospitals in 1973. It is impossible
to estimate the proportions of elderly/long stay patients in
hospitals which were, in the main, acute hospitals.
The London Coordinating Committee
The London Coordinating Committee was established in 1975 to
assist in the solution of these problems. There were long
discussions about how, while remaining an advisory body, it
might be given more bite than Dame Albertine Winner’s joint
working party, which had been active from 1967-72. Its terms of
reference were to ‘coordinate the provision of health services
in Greater London with reference to the matching of medical
education and service need and securing rational distribution of
specialised health services’. The Permanent Secretary, Sir
Philip Rogers, chaired the first meeting. Members were drawn
from the regional health authorities, teaching areas,
postgraduate hospitals, the London Boroughs Association, the
Greater London Council, family practitioner committees, the
University Grants Committee, the University of London and the
Department of Health. It proved to be too large and unwieldy a
body: while it provided a forum for discussion it had neither
the capacity nor the authority to take decisions. It identified
a number of local problems requiring urgent solution. Previous
assessments of regional specialties like neurosurgery and
cardiothoracic surgery were brought up to date and the committee
considered a possible strategy for the rationalisation of inner
London hospitals which had been drawn up by Departmental
officers. The tentative proposals included a suggestion that
some recently completed hospital developments should not be
used for the purpose for which they had been designed, but for
other clinical requirements. The document was leaked in the Sunday
Times creating concern amongst the staff of
some prestigious hospitals.8 The
Minister decided to make the document more widely available in
an attempt to allay anxieties.
Meanwhile
regional authorities, unimpressed by the potential of the London
Coordinating Committee, were coming to believe that their own
planning activities might provide more substantial and
achievable economies. The committee gradually lost favour and
held its last meeting in July 1976. For some time afterwards the
members received briefing about London developments, but few
regretted the committee’s passing. Its ineffectiveness
highlighted the problem of developing London-wide strategies
which would achieve general acceptance. Yet the planning of the
Thames regions was proceeding at widely differing rates, and it
was clear that there would be a variation in comprehensiveness
and quality. Nor would the four plans necessarily be compatible
with each other. Elsewhere in the country this might not have
mattered, but in London, where major reductions in services were
likely to prove necessary and cross-boundary flows were
significant, a measure of coordination was essential.
The London
Health Planning Consortium
For these reasons approaches were made in 1977 to the four
Thames regions, the University of London and the University
Grants Committee. It was agreed that responsibility for health
service planning rested with the regions, but some matters
required the assistance of the university and medical schools,
and others a uniformity of approach. The regions retained their
reservations about the effectiveness of London-wide groups,
unless given power to ensure the implementation of decisions,
but accepted that some major decisions like the future of the
postgraduate hospitals were required before regional strategic
plans could be finalised. It was agreed that the proposed group
would only consider those issues requiring a London-wide
approach, and the London Health Planning Consortium was formed
at the end of 1977 to ‘identify planning issues relating to
health services and clinical teaching in London as a whole, to
decide how, by whom and with what priority they should be
studied; to evaluate planning options and make recommendations
to other bodies as appropriate; and to recommend means of
coordinating planning by health and academic authorities in
London'.
Dame Albertine Winner had retired from the civil service before
becoming the chairman of the Joint Working Group in 1967. The
Consortium, on the other hand, was chaired by a serving
departmental officer, Mr J C C Smith, and received considerable
support in the analytic work required from the Department of
Health. The membership included officers and representatives of
the four Thames regions, the University of London and the
University Grants Committee, the postgraduate hospitals and the
Department itself. It was not an executive body and decisions
continued to lie with the statutory health and academic bodies,
and where necessary with Ministers.6 Concurrently
the University of London was under increasing financial
pressure. To begin with it had not believed that it would
experience financial cuts, although prepared to consider how
best to maintain the quality of its medical and dental education
with so many clouds upon the horizon. The position worsened and
the principal of the university had to ask the deans how they
were not going to spend the money they were not going to get.
The Flowers working
party
In 1977, at the request of the University’s Joint Medical
Advisory Committee, the Conference of Metropolitan Deans set up
a working party to consider rationalisation. However this group
was unable to produce definitive recommendations even though
there was an acceptance of the need for change, and that the
number of medical schools might need to be reduced. As a result
the vice-chancellor established a major review of the resources
for medical and dental education in February 1979. It was
chaired by Lord Flowers, rector of the Imperial College of
Science and Technology. Lord Flowers’ working party started to
meet some time after the London Health Planning Consortium, and
it had to work to a tight timescale. Basic assumptions were that
the current intake of students and the existing level of funding
would be maintained, but that regard should be paid to
demographic trends and the Department of Health’s resource
allocation policy.
The Consortium’s reports
The London Health Planning Consortium faced two main problems.
It was widely accepted that there were many small and medium
sized units in specialties like cardiac surgery and
radiotherapy, and a degree of rationalisation was desirable. The
second problem was the need to reduce the level of acute
hospital services in central London, to bring it into line with
population and with the money likely to be available in the
future. J C C Smith, the Department Under-Secretary, established
a multi-disciplinary group of Department officials who were
smart, enthusiastic and enjoyed skunk work. They drove the
reports and provided the secretariat for the Regional
specialties studies. These were examined by groups with an
independent chairman, specialist expertise being supplied by
people who worked outside London and were less likely to be parti
pris, whilst local knowledge of the London hospitals was
available from consultants working in fields other than the one
under examination. Between 1979-1980 a series of reports were
published for consultation.
The level of acute services was
assessed by examining such factors as the demographic change in
population predicted over a decade, 1978 - 88, taking account of
changes in the distribution of population and its age structure,
hospital utilisation, admission categories, turnover interval
and length of stay. Account was also taken of the extent to
which people from outer London and beyond made use of hospitals
in central London, some of the difficulties posed by social
deprivation in inner London, and the shortcomings in London’s
non-acute services. This work was published in 1979 as a profile
of acute hospital services.10 It showed
how the progressive movement of population outwards had led to a
marked inequality of access to acute services in the Thames
regions, and - in
service terms - to
an over-concentration in central London. The study showed that
there might need to be reductions of the order of 20-25 per cent
in the number of acute beds, amounting in central London to cuts
of around 2,300 beds in all. The consortium suggested that if
this did not happen the health authorities in London would not
be able to find the resources to improve the standard of
services outside the acute sector, in the fields of geriatrics,
mental illness and mental handicap.
Changes of the order suggested would
be bound to have major implications for the medical schools. The
consortium proceeded to study the problem of providing
sufficient clinical facilities for medical education, in
parallel with the work of Lord Flowers’ working party. Two
Department officers, Steve Godber and Geoffrey Rivett, visited
all the deans of the London Medical Schools, to learn the size,
type, and specialty mix that schools needed for their student
intakes. Both groups published their reports on the same
day in February 1980. The consortium’s document, Towards
a Balance, suggested a pattern of hospitals
within which it would be possible to implement a variety of
educational options. It indicated ways in which complementary
hospitals in outer London, which were less affected by declining
population, might be linked with the various medical schools and
used for core teaching in medicine and surgery.
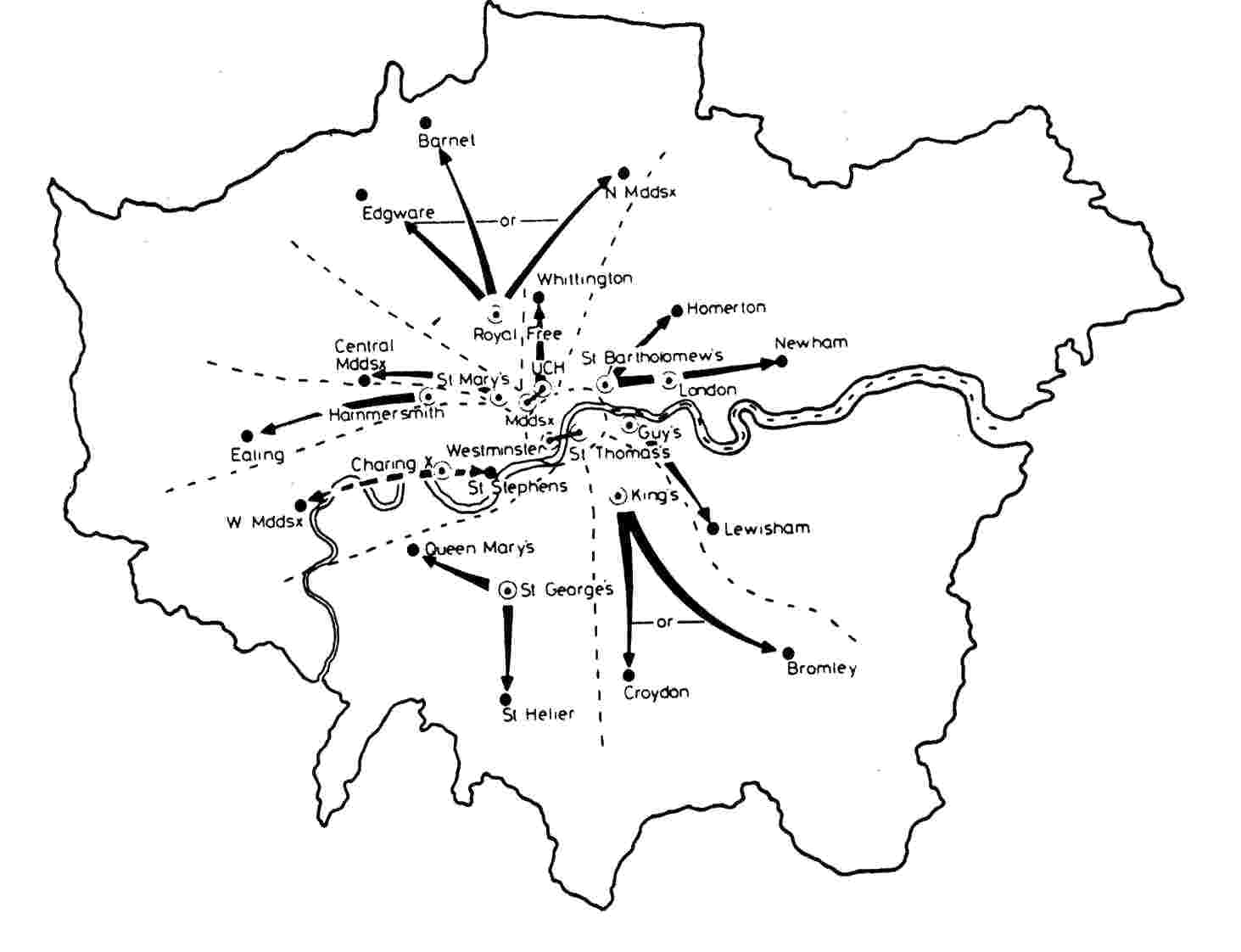
Towards a
Balance: relationship of teaching hospitals to large hospitals
in outer London. Source - Flowers Report and BMJ
8 March 1980. This
edition of the BMJ contains several articles on London hospital
planning
After the
publication of Lord
Flowers’ report it was discussed at a
conference at Senate House.9 Students
from the Westminster Hospital, parading with coffins, made their
views clear. The report suggested that there was over-capacity
in pre-clinical provision, and regarded it as axiomatic that the
University should use new buildings to the full, particularly as
these often lay in areas which remained predominantly
residential. A series of amalgamations was proposed as a result
of which 34 separate academic institutions would be grouped into
six schools of medicine and dentistry, some named after famous
doctors like Harvey and Lister. One protagonist suggested that
it was necessary to overcome ‘tribal loyalties’, a remark which
merely united the tribes in opposition.
A British
Medical Journal editorial expected that there
would be wide protest, indeed that "the the protests from each
institution under threat will merge into an unintelligible
Babel." Amongst the most controversial recommendations
were the closure of the pre-clinical school at King’s College,
Strand, and Westminster Medical School.9 Both
were bitterly and effectively opposed. Faced with such
opposition the University could not come to immediate decisions,
even though financial cuts were inevitable. The conflict spread
wider than the medical faculty, for there were consequences
affecting other institutions. In any case some recommendations
did not seem viable and the University’s joint medical advisory
committee produced a revised plan for restructuring London
medical and dental education which was likely to achieve wider
support. The modifications were accepted by the university joint
planning committee, but the Senate was divided and referred them
back. There was to be further delay. A new working party was
established chaired by the deputy vice-chancellor, Professor
Leslie Le Quesne, to examine the costs and savings which would
result from different patterns of closure and amalgamation.12 The
University employed management accountants to assist with this
costing exercise and in the meanwhile it encouraged those
schools wishing to proceed with closer association to do so.
The costing study necessarily made a number
of assumptions, some of which were open to challenge. In general
the high cost of running the newly built medical schools was
confirmed. Merging medical schools appeared to be more
cost-effective than merely phasing out a preclinical school. It
was also clear that agreement would not be achieved purely by
demonstrating that some solutions were cheaper than others.
Rationalisation in London and
changes in the organisation of medical education were now
overtaken by the events which led to the restructuring of the
National Health Service as a whole in 1982. The ever increasing
demand for resources and the financial problems arising from a
deteriorating economic situation were responsible for some
disillusion following the 1974 reorganisation. By 1976 there was
mounting criticism of a number of its aspects, particularly of
what many felt to be an unnecessarily complex and cumbersome
administrative structure. As a result the Labour government
established a royal commission which carried out an extensive
and wide-ranging study of the health service. It reported in 1979.13 The
Conservative administration which took office in May of that
year formally welcomed the report, but rejected one of the major
recommendations, previously proposed by three of the regional
chairmen, that regions should be accountable to Parliament for
matters within their competence. The proposal for an independent
enquiry into the health service in London was also rejected on
the ground that many of the issues were already under study by
the London Health Planning Consortium.
In general however the government
accepted recommendations aimed at improving and simplifying the
management and organisational structure of the health service. A
discussion document, Patients First, was
issued in December 1979, setting out proposals for the
simplification of the structure by removal of the area tier of
health authorities, which intervened between regions and health
districts, and for the strengthening of unit management by
greater delegation of authority to the operational level.
Instead, district health authorities were proposed, modelled on
existing ‘single district areas’ which had generally been judged
more effective than the areas which had the task of managing
several competitive districts.14 Internal
faction had been characteristic of a number of the area health
authorities in London.
The structure now envisaged would place the managing
authorities, the districts, close to the point of service
delivery, while maintaining regional
authorities for the purposes of strategic planning and resource
allocation. Patients First stated
that in London the government did not contemplate major changes
in regional boundaries in the next few years - in other words
the starfish arrangement would persist and a central London
health authority was not under consideration. It was also
suggested that there would be advantages in the establishment of
an advisory group, representative of major interests, to assist
the government in considering major issues in London.
In May 1980
the Secretary of State established this as the London Advisory
Group, chaired by Sir John Habakkuk (Principal of Jesus College,
Oxford; vice-chancellor of Oxford University, 1973-7) to report
to him and advise on the development of London’s health
services, and the restructuring of health authorities.15 Its
first task was to suggest guidelines for determination of
boundaries in London, a problem recognised as more complex than
elsewhere in the country. These appeared as an appendix to a
departmental circular on structure and management (HC(80)8). Two
further reports published early in 1981 proposed a strategy for
the future organisation of acute hospital services in London.15 They
recommended a reduction in the number of acute beds to free
resources for the elderly, the mentally ill and handicapped, and
for a variety of community services. The London Advisory Group
accepted the conclusions of the London Health Planning
Consortium, after examining its assumptions.
The
consortium had pointed to over-provision in relation to future
needs and had predicted that because of shortening length of
stay the same number of people could be treated in fewer beds.
The group reported that in two years that had elapsed since the
consortium’s calculations there had already been a reduction of
1,950 acute beds, nearly seven per cent, a more rapid rate of
decline than the consortium had projected.
Acute beds
in inner London
|
1977 |
28,600 |
|
|
1979 |
26,650 |
- 6.8
% |
|
1980 |
25,000 |
-
12.6 % |
|
LHPC target for 1988 |
22,500 |
-
21.3 % |
In contrast
to this fall the number of beds in private hospitals in inner
London was rising, more than doubling between 1977 and 1983 to
over 1,300. Some of the private hospitals were themselves
specialising, providing particular facilities like radiotherapy
or maternity and child care.
One of the
most significant statements made by the London Advisory Group
was that full use should be made of major hospitals, reductions
when necessary being made elsewhere, presumably in smaller
institutions. One region, North East Thames, had already been
pursuing this strategy, rationalising smaller hospitals and
building larger district general hospitals at Newham and
Homerton. This approach, which promised to free resources for
other uses, received the general endorsement of the Secretary of
State. Both economic
problems and the appreciation that London had more hospital beds
than could be justified led to a series of closures of small
hospitals where the accommodation was poor and other hospitals
nearby could pick up the load. As an example, in east
London, the Connaught Hospital was closed in 1977, the site
being sold in 1979 for £365,000. There were many
others including Poplar and the South London Hospital for Women,
the closures often being hard fought.
Major
hospitals of which full use should be made15
|
Charing Cross Hospital
|
Lewisham Hospital
|
St
Andrew’s, Bow
|
St
Stephen’s Hospital
|
|
Dulwich Hospital
|
The
London (Whitechapel and Mile End)
|
St
Bartholomew’s Hospital
|
St
Thomas’s Hospital
|
|
Guy’s
Hospital
|
Middlesex Hospital
|
St
Charles’ Hospital
|
University College Hospital
|
|
Hammersmith Hospital
|
Newham Hospital
|
St
George’s Hospital
|
Westminster Hospital
|
|
Homerton (Hackney)
|
Queen
Mary’s, Roehampton
|
St
James’ Hospital, Balham
|
Whittington (Royal Northern)
|
|
King’s College Hospital
|
Royal
Free Hospital
|
St
Mary’s Hospital, W2
|
|
Districting
The regions
were asked to submit proposals for the boundaries of the new
district health authorities to be established, taking the
guidance of the London Advisory Group into account. Because of
the tendency to propose a district to match every viable
district general hospital, the number of authorities created
proved to be considerable. At the Secretary of State’s request
the London Advisory Group considered the submissions. Work was
hampered by the fact that the University of London had not come
to final conclusions on the Flowers report. This was
particularly significant in the centre of London where hospital
catchments seldom matched local authority boundaries, and the
main academic institutions were sited. No ideal arrangement was
possible in inner London, whereas in outer London there were few
problems and in the main the regions’ proposals were accepted.15
The
university was considering the association of the medical
schools of Charing Cross and the Westminster Hospitals, which
led the North West Thames region to propose the establishment of
a single district to be known as ‘Riverside’ to be responsible
for both teaching hospitals. The university also suggested that
the medical schools of the Royal Free Hospital, University
College Hospital and St Mary’s should be grouped together. This
commanded little support in the committee established to
consider the proposition, all three medical schools preferring a
pairing which excluded St Mary’s. This opened another
possibility, a joint district to be known as Bloomsbury, to
manage the Middlesex and University College Hospitals. The two
teaching hospitals were close to each other, but lay on opposite
sides of a regional boundary and the idea was initially opposed
by the hospitals, the regions and the university.
The Secretary
of State was concerned to find a balance between the conflicting
requirements of coterminosity and practicability in health
service terms. His decisions differed in some respects from the
recommendations of the London Advisory Group.15 In
only one case was a district established which contained more
than one teaching hospital, Bloomsbury. Much work had gone
on behind the scenes over the previous months; the suggestion of
the amalgamation of the medical schools had been raised by
Department officers with the Deans of UCH and the Middlesex
Medical Schools and they had spoken to each other and the staff.
The University had been consulted and when it was clear that the
amalgamation was possible the Deans had seen the Secretary of
State. Similarly, off-the-record discussions took place with
Deans of the general teaching hospitals about the integration of
smaller postgraduate medical schools. The Westminster,
sure that it was secure, refused to consider turning itself in
part to a postgraduate centre. St Thomas' preferred
dermatologists to urogenital surgeons. Once the decisions were
announced they were accepted with good grace and an evident
desire to take advantage of the consolidation of two
undergraduate teaching hospitals and three postgraduate groups,
St Peter’s, the Royal National Orthopaedic and the Royal
National Throat, Nose and Ear hospitals. The grouping gave the
Bloomsbury district authority a worthwhile management task and
avoided the risk of separate authorities each bent on the
defence of its own institutions. In London as a whole
coterminosity remained a major feature. 27 out of 33 London
boroughs related to only one district and 18 were coterminous
with the matching health authority. Feelers to other
medical schools put out by the Department showed that the ground
was not fertile for other amalgamations.
With the
publication of the London Advisory Group’s last report its work
was complete, and it was disbanded in 1981 at the same time as
the London Health Planning Consortium.
The
decisions of the University of London
In December
1981, a year in which the University Grants Committee announced
a reduction in grant in each of the next three years, the
University of London finally reached conclusions on the pattern
of undergraduate medical education in London.17 It
was decided to reduce the number of separate schools, only four
remaining independent; the Royal Free, St Mary’s, St George’s
and King’s College Hospital Medical School which was in any case
uniting with King’s College Strand. Charing Cross and the
Westminster Medical Schools would be strengthened by merger; the
proposal by the medical schools of Guy’s and St Thomas’s to form
the United Medical Schools under a single governing body was
supported; the medical colleges of St Bartholomew’s and The
London should cooperate; and a joint school would be established
between the Middlesex and the Faculty of Clinical Sciences of
University College. The last would mirror Bloomsbury, creating
an academic organisation of considerable size and prestige. The
newly constructed medical school buildings at St George’s and
Charing Cross had proved expensive to run, largely because they
provided a much higher standard of accommodation. But they were
sited further from central London in the midst of large
residential areas, and it seemed only sensible to exploit this
advantage.
The
governance of the postgraduate hospitals
The
governance of the specialist postgraduate hospitals had been put
to one side in 1974. It was difficult to see where they might
best fit in to the reorganised health service. The 1972
reorganisation White Paper suggested that they should become
closely associated with other services in their vicinity, in
line with the recommendations of the Royal Commission on Medical
Education in 1968.18 The existing boards
of governors were preserved and continued to function under
earlier health service acts.
The old
antipathies between the specialist hospitals, which often formed
the focal point of a specialty unable to claim many beds within
a general hospital, and the undergraduate hospitals, persisted
in the form of a mutual wariness. The association suggested in
the White Paper had little appeal for the postgraduate
hospitals, which had branches in several parts of London and
seldom related clearly to a single region. To become too closely
involved with a general hospital carried the risk of merger and
ultimate extinction. Nevertheless, their future role required
examination and in 1976 the university established a working
party under the chairmanship of Professor Norman Morris to
review the academic institutes with which the postgraduate
hospitals were associated.
In March
1976, Dr David Owen suggested that a single authority might
integrate the planning and management, and rationalise the
services of three hospitals which lay next to each other: the
Hospital for Sick Children, Great Ormond Street, the National
Hospital for Nervous Diseases, and the Royal London Homeopathic
Hospital. A steering committee accepted the possibility of such
an arrangement, while pointing out the difficulties and
complexities which would be involved. Incorporation of
postgraduate hospital groups into area health authorities was
another possibility. The postgraduate hospitals made it clear
that the onus of justifying change lay upon those proposing it.
Led by Sir Reginald Wilson, the boards pointed out that their
activities spread far wider than the boundaries of any one
district, and some groups managed hospitals in two or three
different regions. They denied that planning arrangements with
the regions were inadequate, were well satisfied with the status
quo, and preferred to maintain their direct link with the
Department of Health and Social Security.
In September
1978 after several meetings and conferences, the Department
issued a discussion document which proposed the establishment
of a London postgraduate health authority.19 This
would take over the Department’s role in planning and resource
allocation, but would remain directly responsible to the
Secretary of State. The existing boards of governors would
remain in place for the time being. Other options were also
canvassed which involved the early disappearance of the boards,
but in the absence of consensus the DHSS preferred to temporise.
The proposal for an ‘overlord’ postgraduate health authority was
regarded by the hospitals as very much second best; they
preferred the status quo. The idea was criticised in the House
by Mr. Patrick Jenkin as the insertion of a further tier of
management when simpler structures were in fact required.
Shortly afterwards, in May 1979, a Conservative government was
elected and Mr. Jenkin became Secretary of State for Social
Services. It was then decided to take no action until reports of
the Flowers working party9 and the Royal
Commission on the National Health Service13 were
available.
The London
Advisory Group considered the management arrangements of the
postgraduate hospitals in 1980 and visited all of them. The
university was considering the possibility of merging some
institutes with medical schools, but where it proposed to
maintain a separate university institute this argued for the
maintenance of an independent authority. The presence of
university representatives on the London Advisory Group was
therefore important, so that all could be made aware of the way
university thinking was developing. In its report, the London
Advisory Group distinguished between hospitals which were to be
rehoused in close association with general hospitals, or where
the matching institute was likely to be merged with a general
medical school as a result of the decisions following the
Flowers report; and those which were unlikely to move from their
existing sites and where the institute was likely to continue in
its present form for the foreseeable future.15 It
recommended that the first group should be managed by the
appropriate district health authority from 1 April 1982.
Hospitals in the second category, in general the larger ones
with more viable institutes, should be managed by newly
established special health authorities in place of the existing
boards of governors. Following consultation, the Secretary of
State established special health authorities for six groups, and
for the Hammersmith Hospital. The Hospitals for Sick Children,
the Royal Marsden, the National Hospitals for Nervous Diseases,
Moorfields, Bethlem Royal and Maudsley, and the National Heart
and Chest Hospitals, remained independent of the regional health
authority structure. The Hammersmith, associated with the Royal
Postgraduate Medical School, while wishing to remain accountable
to the North West Thames region, found to its surprise that it
was reconstituted as a special health authority. Department
officers visited teaching hospitals such as St Thomas', the
Westminster and the Middlesex, trying to find an appropriate and
willing partner that would maintain the excellent features of
these small posstgraduates. The advantages of taking on a unit
of prestige - and its budget - were not lost on some hospitals,
and St Thomas' was a willing host for the skin hospitals.
Others, such as the Westminster, felt they were in need of
neither advice, nor help, nor a new unit and lost the
opportunity. Four groups came under the
management of a district authority: the Royal National
Orthopaedic Hospitals, the Royal National Throat, Nose and Ear
Hospitals, the St Peter’s group and St John’s Hospital for
Diseases of the Skin. The first three came under Bloomsbury, and
St John’s under West Lambeth where it was likely to be relocated
(within St. Thomas' Hospital).16 Decisions
on the Eastman Dental Hospital and Queen Charlotte’s were
postponed.
During the
months preceding the restructuring of the health service on 1
April 1982, chairmen and members were selected for the new
district authorities and new officer teams were appointed. Once
again management was to operate by consensus. Certain teaching
districts were designated: those deeply involved in medical
education because they managed the main university hospital used
by a medical school.20 Some of the
medical schools prepared the private legislation needed to unite
independent institutions, in line with the university’s
proposals.
The pattern
of the acute services was changing; small hospitals were
closing, small accident and emergency departments were
disappearing. Evolution was assisted in some places, like
Bloomsbury, by the way in which restructuring changed the
responsibilities of authorities. Amalgamation and
rationalisation, the chosen tools of the King’s Fund in earlier
years, were once more the order of the day. Health authorities
now, for financial if for no other reasons, had to grasp the
nettle of reshaping the hospital services in central London more
closely to national priorities. The pace of change was
increasing, major hospitals felt threatened, and in fighting for
survival might urge the closure of competitors. King's
College Hospital, in particular, was under assault..
1 Machiavelli
N. Il Principe. Rome, Antonio Blado, 1532.
2 Great Britain, Parliament. National
Health Service reorganisation: England. London, HMSO, 1972. Cmnd
5055.
3 Great Britain, Department of Health
and Social Security. Management arrangements for the reorganised
National Health Service. London, HMSO, 1972.
4
Great Britain, Department of Health and Social Security. The NHS
planning system. London, DHSS, 1976; Great Britain, Department
of Health and Social Security. Priorities for health and
personal social services in England: a consultative document.
London, HMSO, 1976; and Great
Britain, Department of Health and Social Security. The way
forward: further discussion of the Government’s national
strategy based on the consultative document - Priorities
for health and personal social services. London, DHSS, 1977.
5 Great Britain,
Department of Health and Social Security. Sharing resources for
health in England: report of the resource allocation working
party. London, HMSO, 1976; and Ranger
D. RAWP. University of London Bulletin no 41, May 1977.
6
Great Britain, Department of Health and Social Security. On the
state of the public health. Annual report of the Chief Medical
Officer for 1979. London, HMSO, 1980; The Times, 26 February
1980; and British
Medical Journal, 1980, i, p 723.
7 Joint survey of medical and surgical
services in the county of London. London, P and S King and
London County Council, 1933.
8 Rationalisation of services: a revised
hospital plan for inner London. London Co-ordinating Committee,
1975. (LCC(75)13); Sunday Times, 23 November 1975; and Hospital
and Health Services Review, February 1976.
9 London
medical education. A new framework: report of a working
party on medical and dental teaching resources. (Chairman: Lord
Flowers). London, University of London, 1980; University of
London press release, February 1979.
10 London Health Planning Consortium. Acute hospital
services in London. London, HMSO, 1979.
11 London Health Planning Consortium. Towards a
balance. London, DHSS, 1980; and British Medical Journal, 1980,
i, pp 665-6, 734-5.
12 Great Britain, Department of Health and Social
Security. On the state of the public health. Annual report of
the Chief Medical Officer for 1980. London, HMSO, 1981.
13 Royal Commission on the National Health Service.
Report. (Chairman: Sir Alec Merrison). London, HMSO, 1979. Cmnd
7615.
14 Great Britain, Department of Health and Social
Security and Welsh Office. Patients first: consultative paper on
the structure and management of the National Health Service in
England and Wales. London, HMSO, 1979.
15 Reports of the London Advisory Group. London,
1981.
1 Acute
hospital services in London;
2 District
health authorities in London;
3 Management
arrangements for the postgraduate specialist teaching hospitals;
4 The
development of health services in London.
16 Great Britain, Department of Health and Social
Security. On the state of the public health. Annual report of
the Chief Medical Officer for 1981. London, HMSO, 1982.
17 Joint planning committee of the University of
London on medical education in London. Report. London,
University of London, 1981.
18 Royal Commission on Medical Education 1965-8.
Report. (Chairman: Lord Todd). London, HMSO, 1968. Cmnd 3569.
19 Great Britain, Department of Health and Social
Security. The future management of the London specialist
postgraduate hospitals. London, DHSS, 1978.
20 The membership of district health authorities,
HC(81)6 Appendix 5; see also HC(82)2 Appendix 2.
|